Arsenic Exposure Assessment for the Arizona Hopi Tribe

SWEHSC Members Highlight: Mary Kay O’Rourke, Jefferey Burgess, Robin Harris
Summary:
The Hopi Tribe is a sovereign nation located in rural northeastern Arizona, where health disparities, public concern about arsenic exposures, and limited exposure assessment are prevalent. Arsenic is a naturally occurring metalloid (an element with metal and non-metal chemical and physical properties) found in the earth’s air and water that is associated with multiple adverse health outcomes. To assess and combat arsenic exposure levels among the Hopi Tribe, the Hopi Environmental Health Project was established under the leadership of Drs. Jefferey Burgess, Robin Harris, and Mary Kay O’Rourke, members of the Southwest Environmental Health Sciences Center (SWEHSC) and faculty at the Mel and Enid Zuckerman College of Public Health (MEZCOPH).
Working with members of the Hopi Tribe, this project recruited 76 households throughout Hopi lands and conducted chemical analyses to assess arsenic levels in various water sources at two different time points. The team also administered questionnaires for a more comprehensive understanding of participants’ usual food intake. During both heating (November-May) and non-heating (June-October) seasons, arsenic exposure from food was greater than exposure from other sources, such as water or inhalation of dust or smoke from heating stoves. This study highlights the importance of continued investigation and assessment of exposure routes to harmful metalloids to ensure the protection of health in vulnerable populations.
Introduction:
The Hopi Tribe is a sovereign nation located in rural northeastern Arizona, where health disparities, public concern about arsenic exposures, and limited exposure assessments are prevalent. Arsenic is a naturally occurring metalloid (an element with metal and non-metal chemical and physical properties) found in the earth’s air and water that is associated with multiple adverse health outcomes with long term exposure to high levels of arsenic.
To assess arsenic exposure levels through multiple potential exposure routes, the Hopi Environmental Health Project was established under the leadership Robin Harris and Mary Kay O’Rourke, members of the Southwest Environmental Health Sciences Center (SWEHSC) and faculty at the Mel and Enid Zuckerman College of Public Health (MEZCOPH). The first author Adam Carl and co-author Jonathan Bloom began working on this project as part of the NIEHS-funded Environmental Health Sciences – Transformative Research Undergraduate Experience (EHS-TRUE). Dr Carl went on to obtain his MS in Environmental Health Sciences at MEZCOPH and to graduate with an MD from the University of Arizona (UA). Dr. Carl speaks about his work in empowering the next generation of Native American physicians in this article: https://healthsciences.arizona.edu/news/blog/meet-medical-student-paying-it-forward. He was raised at Hopi and is a member of the Navajo Nation, which he speaks about on the KXCL Radio for their “Thesis Thursday” podcast, which can be found here: https://kxci.org/podcast/adam-carl/. A third co-author Steven Hadeed completed his PhD at MEZCOPH and was a NIEHS T32 predoctoral fellow.
This project was a part of the Center for Indigenous Environmental Health Research (CIEHR) at the University of Arizona, supported by the supported by the National Institute of Health’s National Institute of Environmental Health Sciences and the Environmental Protection Agency (NIEHS) and directed by co-author, SWEHSC member and MEZCOPH professor, Jeff Burgess, MD, MS. SWEHSC member.
What were the methods of data collection and analysis?
In 1995, members of the University of Arizona research team began collaborating with Hopi partners on cancer screening and prevention initiatives. Over time, tribal partners began to express concerns about the increasing prevalence of asthma, as well as exposure to arsenic and uranium from water, and toxins migrating from landfills. To address these issues, the Hopi Environmental Health Project was conducted from 2016 to 2020. Potential households were identified spatially using Google Earth with 222 potential housing structures randomly selected, of which 126 were eligible and 76 households were enrolled in the study. These households were distributed across Hopi land in proportion to the population of each village relative to the tribal population. All protocols and consenting documents were approved by the UA Institutional Review Board. In addition, the project was approved by the Hopi Tribal Council. A Community Advisory Board reviewed all procedures, and all local research staff were members of the Hopi Tribe and living at Hopi. A large contribution to this project involved training local tribal interviewers, field technicians, and community health representatives (CHRs) to implement the project design, collect data, and build capacity for independent tribal research projects.
Each house was investigated during both the heating and the non-heating season to evaluate differences in activities, home ventilation, diet, fuel use, and other factors. The heating season runs from early November through early May, while the non-heating season runs from June through early October. Participants also completed questionnaires to share data regarding their demographics, housing characteristics, and diets. Samples sent to the Arizona Laboratory for Emerging Contaminants (ALEC), a SWEHSC facility core, for chemical analysis of arsenic included: air, water, soil, house dust, and urine. In addition, this study analyzed different exposure factors, such as time spent indoors versus outdoors and water/food ingestion, to create a better understanding of the chemical analysis.
What were the results of the study?
The figures below show the contribution of various sources (food, water, and inhalation) to the Hopi participants’ Arsenic Daily Dose (ADD) during heating (Figure 1) and non-heating seasons (Figure 2). Dietary ingestion contributed the greatest proportion to the aggregate ADD of arsenic for both heating and non-heating seasons, whereas soil ingestion outside of homes contributed the smallest proportion to the aggregate ADD in both seasons.
According to the reported dietary intake, the most consumed food group by participants was breads/starches/snacks (24%), followed by vegetables (21%), beverages (18%), fats and oils (13%), meats and soups (10%), and fruits (3%). Understanding which food groups are consumed most frequently enables researchers to identify and prioritize potential dietary sources of arsenic exposure.
Figure 1.
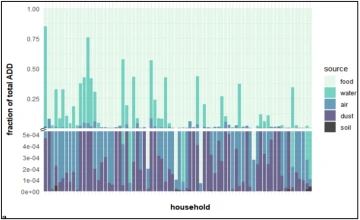
Note: Contribution of arsenic in various media to the average daily dose within the heating seasons. Adapted from “A Multimedia Arsenic Exposure Assessment for the Hopi Tribe, AZ, USA”, by Carl, A.C., Canales, R.A., Blohm, J.E. et al., 2025, Exposure & Health, Volume 17, 847-862.
During the heating season, arsenic exposure from food was approximately 8 times greater than arsenic exposure from drinking water. Additionally, exposure from food was 115 times greater than arsenic exposure from inhalation.
Figure 2.
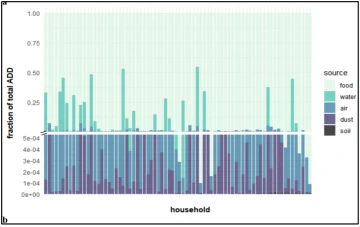
Note: Contribution of arsenic in various media to the average daily dose within the non-heating seasons. Adapted from “A Multimedia Arsenic Exposure Assessment for the Hopi Tribe, AZ, USA”, by Carl, A.C., Canales, R.A., Blohm, J.E. et al., 2025, Exposure & Health, Volume 17, 847-862.
During the non-heating season, arsenic exposure from food was approximately 12.5 times greater than exposure from drinking water. Additionally, arsenic exposure from food was 125 times greater than exposure from inhaled particles. Regardless of the season, the levels of arsenic exposure from food were much greater than exposure from drinking water or inhalation.
What is the importance of measuring metalloid exposure?
Measuring metalloid exposure helps to assess the levels and routes of exposure of harmful chemicals in a specific area. Although arsenic exposure can occur through many routes, this study found dietary ingestion to be one of its primary pathways, through both water and food. Despite high levels of arsenic in the samples of piped water, that value was not reflected in the participants’ urine samples. This is most likely because most participants used bottled water for drinking and cooking. While bottled water can serve as an alternative water source with lower levels of arsenic, it can become expensive and impractical for daily usage. Delivering cleaner water directly to homes can reduce arsenic exposure from piped water, which this study identified as a major source of exposure. Furthermore, the delivery of clean tap water can save residents the cost of purchasing bottled water and ensure safer and cleaner water for Hopi residents.
Although arsenic exposure can occur through several routes, this study highlights ingestion through food as a critical yet often overlooked source. Across both heating and non-heating seasons, arsenic exposure from food exceeded that of other sources. The top five foods associated with elevated levels of arsenic were organ meats (liver, heart, and kidney of various animals), cereals, rice, corn, and legumes (beans, peas, and lentils). These findings suggest that future policy efforts should prioritize reducing arsenic concentrations in food. Minimizing arsenic levels in both food and water is crucial to lowering the intake of toxic metalloids and promoting the health and safety of vulnerable populations.
